Wet AMD accounts for over 10% of all AMD cases, but is responsible for 90% of legal blindness.
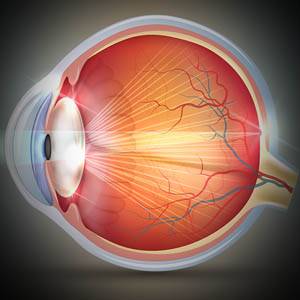
Macular degeneration, also known as age-related macular degeneration (AMD), is an eye disease that occurs as a result of permanent damage to the macula, the center of the retina. Macular degeneration causes loss of central vision and the ability to see fine details. This disease significantly impacts reading, driving, using a computer, watching TV, facial recognition, and many other regular activities.
- Macular degeneration accounts for 8.7% of global blindness.
- Macular degeneration is one of the leading causes of vision loss in adults over the age of 60.
What causes wet AMD?
Wet AMD develops as a result of abnormal blood vessels that form under the retina, and leak blood and fluid into the macula. Wet AMD is the more advanced stage of AMD, with dry AMD usually preceding it.
Dry AMD causes slow progressive damage to the macula. However, once new blood vessels start to grow under the macula, the condition is considered more severe, and is called wet AMD.
There are two main causes of wet AMD:
- Abnormal blood vessel growth. When abnormal new blood vessels grow from the choroid, the space between the retina and the outer layer of the eye (sclera), they tend to grow under and into the macula. These abnormal blood vessels are prone to breaking, and may consequently leak fluid or blood into the macula, causing retinal damage.
- Fluid buildup in the back of the eye. When fluid leaks from the choroid, it can accumulate between the retinal pigment epithelium, a thin cell layer, and the retina. This accumulation of fluid can cause a blister in the macula, and lead to visual distortions or vision loss.
What are the symptoms of wet AMD?
The symptoms of wet AMD occur suddenly, and progress rapidly, causing severe damage and vision loss.
- Central vision loss
- Well defined blind spots in central field
- Visual distortions, such straight lines appearing wavy
- Colors appear less vibrant
- Vision appears hazy
If you have been diagnosed with macular degeneration, contact an eye doctor near you, who can discuss the best options.
SEE RELATED: Dry Macular Degeneration (AMD)
How is wet AMD diagnosed?
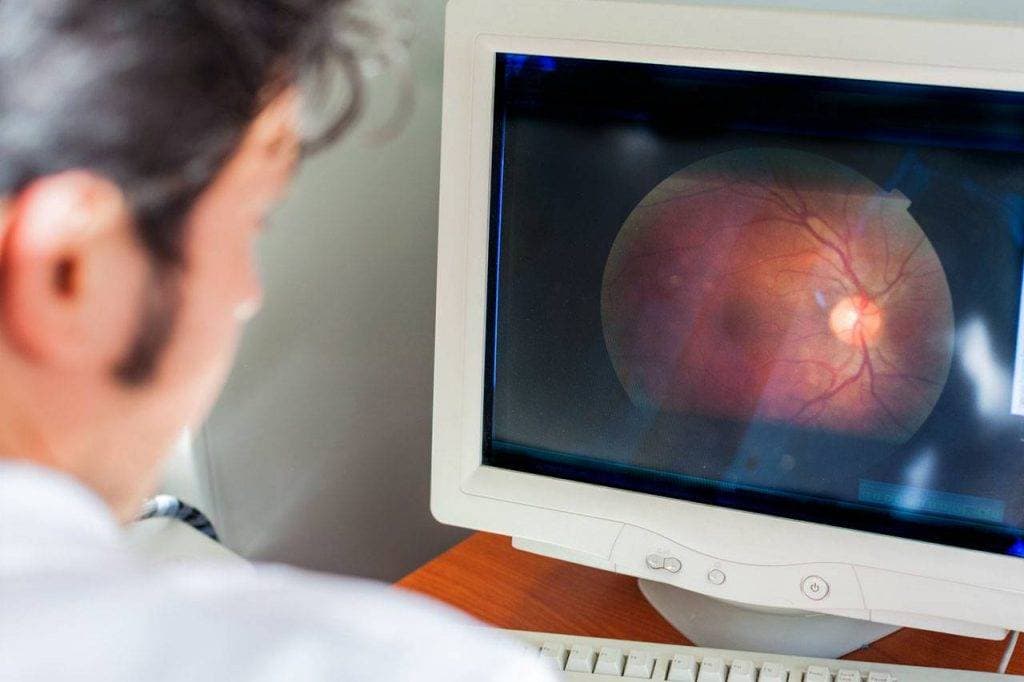
During your eye exam, your eye doctor will perform a series of tests to identify and calculate any retinal damage.
He may utilize any of the following diagnostic tools and assessments:
- Retinal exam. Your eye doctor will dilate your eyes using special eye drops, for a clear view of your retina in the back of your eye. During the exam, your eye doctor will look for fluid or blood and drusen— yellow deposits that form under the retina.
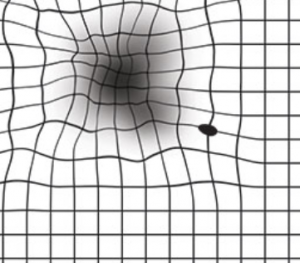
- Test for central vision. Your eye doctor may use an Amsler grid to identify any anomalies in your central vision. If you have AMD, the straight lines in the grid may appear faded, broken or distorted.
- Fluorescein angiography. During this test, a colored dye is injected into a vein in your arm. The dye travels to your retina and highlights any damage to the blood vessels. Your eye doctor will then use a special camera to photograph the dye as it travels through the blood vessels— to facilitate identification of damage or leakage.
- Indocyanine green angiography. Similar to a fluorescein angiography, this test may be used to confirm the results of a fluorescein angiography or to detect abnormal blood vessels in the deeper layers of the retina.
- Optical coherence tomography (OCT scan). This is a noninvasive imaging test that creates a detailed image of the cross sections of the retina. This test enables your eye doctor to detect any areas of the retina that are thinning, thickening or swelling.
How is wet AMD treated?
Treatment of wet AMD can include different methods aimed at stopping the development of new blood vessels, destroying existing blood cells, and preventing fluid from leaking into the macula.
Treatment options for wet AMD include:
- Anti-VEGF treatment
- Laser photocoagulation
- Photodynamic therapy
What is anti-VEGF treatment?
Vascular endothelial growth factor (VEGF) is a protein in your body that produces new blood vessels as your body needs them. Too much VEGF protein in the body will lead to abnormal blood vessels growth. These abnormal blood vessels are prone to breaking and leaking fluid, and can cause retinal damage and permanent vision loss.
Anti-VEGF treatments block the production of the VEGF protein to ensure that only a healthy amount remains in your body.
- 90% of people report stabilized vision after treatment
- 30% of people report improved vision after treatment
1. How is the medication administered?
The anti-VEGF medication is administered through an eye injection, by your eye doctor. Your eye doctor will use an eye numbing agent to prevent any pain during the procedure. A thin needle will then be used to inject the medication into the white part of your eye (sclera).
Injections are usually repeated, based on severity and the patient’s individual needs.
2. Types of anti-VEGF medications
There are different types of anti-VEGF medications— all work in the same way, but use different active drugs:
- Beovu is drug called brolucizumab.
- Avastin is a drug called bevacizumab.
- Lucentis is a drug called ranibizumab.
- Eylea is a drug called aflibercept.
- Mucugen is a drug called pegaptanib sodium.
Laser photocoagulation
Laser photocoagulation surgery seals off the leaking abnormal blood vessels, while preserving the healthy ones. This surgery slows down the progression of further vision loss.
During the procedure, a high-energy laser beam seals off all of the abnormal blood vessels under the macula to stop them from bleeding, and prevent them from further damaging the macula.
The laser that is used during this treatment causes scarring, and can therefore lead to a blind spot within the central field. Also, repeated treatments may be required as blood vessels may reproduce.
Laser photocoagulation is fairly uncommon, as few people with wet AMD are ideal candidates for this procedure. To be an ideal candidate, you cannot have any abnormal blood vessels under the center of your macula, and damage to your macula cannot be too severe.
Photodynamic therapy (PDT)
Photodynamic therapy in an in-office procedure that involves both a laser and medication, called Visudyne dye. The dye is injected into a vein in your arm, and activated when exposed to light.
Prior to the procedure, eye drops will be inserted into your eye to both dilate and numb your eye. After the Visudyne dye is injected, it travels through the bloodstream to the abnormal blood vessels under the retina. In order to activate the light-sensitive dye, your eye doctor will shine a laser into your eye, through a special contact lens. Once the dye is activated, it will work to seal off all of the abnormal blood vessels.
After the procedure, your eyes may feel a bit sore, and you might have some blurry vision. Your eye doctor may cover your eye temporarily to reduce sensitivity.
The effects of the laser are often short-term, so additional procedures may be required.
Low vision devices
Wet AMD may cause permanent central vision loss and can significantly affect your level of independence. However, there are a variety of low vision devices, such as magnifiers, telescopes, hand held devices and computer programs, that can help you to maximize your remaining vision, and enable you to perform many activities for yourself.
Who is at risk of developing wet AMD?
It is important to understand all of the factors that may increase your risk of wet AMD— those out of your control, and those that can be controlled. Controlling certain environmental risk factors can help reduce your chances of developing wet AMD.
The following risk factors are out of your control:
- Age (over age 60)
- Family history
- Race
- Gender (female)
- Light-colored eyes
- High levels of C-reactive protein (CRP), indicating inflammation in the body
- High hyperopia
The following risk factors can be controlled with medication and /or professional support:
- Obesity
- High cholesterol
- Hypertension
- Unchecked cardiovascular disease
- Smoking
- Exposure to ultraviolet (UV) rays
- Certain medications
How can I prevent AMD?
While some risk factors are not in your control, try to incorporate some lifestyle changes to reduce your risk of AMD:
- Quit smoking cigarettes or other tobacco products
- Consume a healthy diet full of vitamins and nutrients
- Create a regular exercise routine— and stick to it
- Maintain healthy cholesterol and blood pressure levels
- Wear sunglasses with 100% UV protection
LEARN MORE: Guide to Eye Conditions
Schedule an eye exam with an eye doctor today— to protect your ocular health, preserve your vision, and enhance your quality of life.
The best way to protect your ocular health is to visit your eye doctor for annual eye exams. Your eye doctor will monitor any changes to your vision and ocular health, and if needed, provide early treatment before vision loss can occur.